Atrial Fibrillation
Learn about AFib, its risks, and management


Atrial Fibrillation Insights
Atrial fibrillation (AF) is one of the most common heart rhythm disorders in today’s healthcare landscape. Affecting over 33 million people globally, it poses significant health risks, such as stroke and heart failure. Accurate diagnosis is crucial for effective treatment and prevention. One essential yet often overlooked method for improving AF diagnosis is the analysis of images generated by electrocardiograms (ECGs) and echocardiograms. This post explores the hidden patterns within these images and how they can aid in the early detection and management of atrial fibrillation.
Atrial fibrillation is marked by irregular heartbeats, which can lead to poor blood flow and increased risks of clot formation. Patients often experience symptoms like palpitations, fatigue, and shortness of breath. In fact, about 25% of patients with AF may be asymptomatic, making accurate identification even more critical.
The underlying electrical disturbances in the heart that cause AF can be visualized using advanced imaging techniques. The prevalence of AF is rising globally; for instance, it affects roughly 1-2% of the overall population, a figure that increases with age—up to 10% in people over 80.
Echocardiography: Going Beyond Electrical Activity
In addition to ECGs, echocardiography provides a vital look at the heart’s structure and function. Utilizing sound waves to create real-time images, this imaging technique allows cardiologists to assess any structural abnormalities contributing to AF.
Identifying Structural Heart Changes
Echocardiograms can unveil significant changes in the heart’s atria, such as dilation or impaired function. For instance, a dilated left atrium not only indicates a higher risk of AF but can also foretell potential complications like stroke. Research shows that patients with left atrial enlargement are five times more likely to develop atrial fibrillation than those with a normal-sized atrium.
Identifying these structural changes early can facilitate timely interventions, potentially preventing the progression of the disease to more severe forms.
Challenges in Interpretation of Imaging Results
Despite advancements in imaging technologies, challenges remain in interpreting results effectively. Variability in AF presentation necessitates a careful approach in analyzing these images.
The Need for Standardization
The interpretation of ECGs and echocardiograms can differ significantly among practitioners, leading to potential misdiagnosis or delayed treatment. Establishing standardized guidelines and providing training for healthcare professionals is vital for ensuring consistent and accurate image analysis. By integrating advanced technology with traditional diagnostic methods, we can bridge gaps in interpretation, ultimately enhancing patient outcomes.
Future Prospects in Imaging Technologies
The field of imaging for atrial fibrillation is on the brink of groundbreaking innovations. Technologies like wearable devices for continuous heart rhythm monitoring are already emerging.
Moving Toward Better Diagnosis and Management
The images associated with atrial fibrillation—whether from ECGs or echocardiograms—provide invaluable information essential for accurate diagnosis and treatment. By uncovering hidden patterns through advanced analysis, healthcare professionals can significantly improve patient outcomes.
A commitment to enhancing physician skills in interpreting these images, combined with advancements in imaging technologies and AI, sets a positive course for the future. As we explore the complexities of atrial fibrillation, embracing these technological advancements can lead to more personalized and effective care for individuals at risk of this serious condition.
The path toward better diagnosis of atrial fibrillation relies on our ability to analyze and interpret these images effectively. Continued efforts may reveal even more ways to understand this condition, ensuring optimal care is accessible for all patients.
The Role of ECG in Diagnosing Atrial Fibrillation
Electrocardiograms are the primary imaging tool for diagnosing atrial fibrillation. An ECG records the heart’s electrical activity, allowing healthcare professionals to spot abnormalities indicative of AF. A standard 12-lead ECG can reveal key features, such as the absence of consistent P waves and irregular ventricular responses.
Hidden Patterns in ECG Readings
When analyzing ECG readings for AF, attention to detail is essential. A common hallmark to look for is the “irregularly irregular” rhythm associated with AF. By examining the intervals between beats, healthcare providers can identify subtle differences that may go unnoticed.
Recent advancements in artificial intelligence (AI) have further revolutionized ECG analysis. AI algorithms can be trained to recognize unique signatures of atrial fibrillation, improving the speed and accuracy of diagnoses. For example, studies show that AI can increase sensitivity in detecting AF by over 15%, which could lead to improved patient outcomes.
Atrial Fibrillation Insights

Explore comprehensive information on atrial fibrillation and its symptoms and risk factors
Symptoms of Atrial Fibrillation
Not everyone with AFib experiences symptoms, and some may only have occasional episodes, but common symptoms include:
Risk Factors for Atrial Fibrillation
- Palpitations: A sensation of the heart beating rapidly or irregularly. Some people describe it as a fluttering or pounding in the chest.
- Fatigue: Feeling unusually tired or weak, even after getting enough sleep.
- Shortness of breath: Difficulty breathing, especially with physical exertion or when lying down.
- Dizziness or lightheadedness: Feeling faint or unsteady, which can be related to irregular blood flow to the brain.
- Chest pain or discomfort: This can occur in some people, though it’s more common in those with underlying heart disease.
- Difficulty exercising: The irregular heart rhythm can lead to reduced exercise tolerance.
- Confusion or difficulty concentrating: Decreased blood flow to the brain can affect cognitive function, particularly in older adults.
Several factors increase the likelihood of developing AFib, including:
- Age: The risk increases as you get older, especially after age 60.
- High blood pressure (Hypertension): Chronic high blood pressure can damage the heart and increase the risk of AFib.
- Heart disease: Conditions like coronary artery disease, heart valve problems, heart failure, or a history of heart attacks increase AFib risk.
- Previous stroke or transient ischemic attack (TIA): If you’ve had a stroke or TIA (mini-stroke), you’re at higher risk for AFib.
- Diabetes: Having diabetes increases the risk of AFib, especially if it’s poorly controlled.
- Obesity: Being overweight or obese places extra strain on the heart, raising the risk of AFib.
- Sleep apnea: Obstructive sleep apnea, which causes breathing to stop and start during sleep, is linked to an increased risk of AFib.
- Family history: If someone in your family has had AFib, your risk may be higher.
- Alcohol consumption: Heavy drinking, or even occasional binge drinking (often referred to as “holiday heart syndrome”), can trigger AFib episodes.
- Thyroid problems: An overactive thyroid (hyperthyroidism) or other thyroid disorders can increase the risk of AFib.
- Chronic lung disease: Conditions like COPD or emphysema can increase your risk due to the strain they put on the heart.
- Stress or excessive caffeine intake: In some cases, prolonged stress or excessive intake of stimulants like caffeine can trigger AFib.
- Infections or illness: Severe infections or illness that stress the body (such as pneumonia or COVID-19) can sometimes lead to AFib.

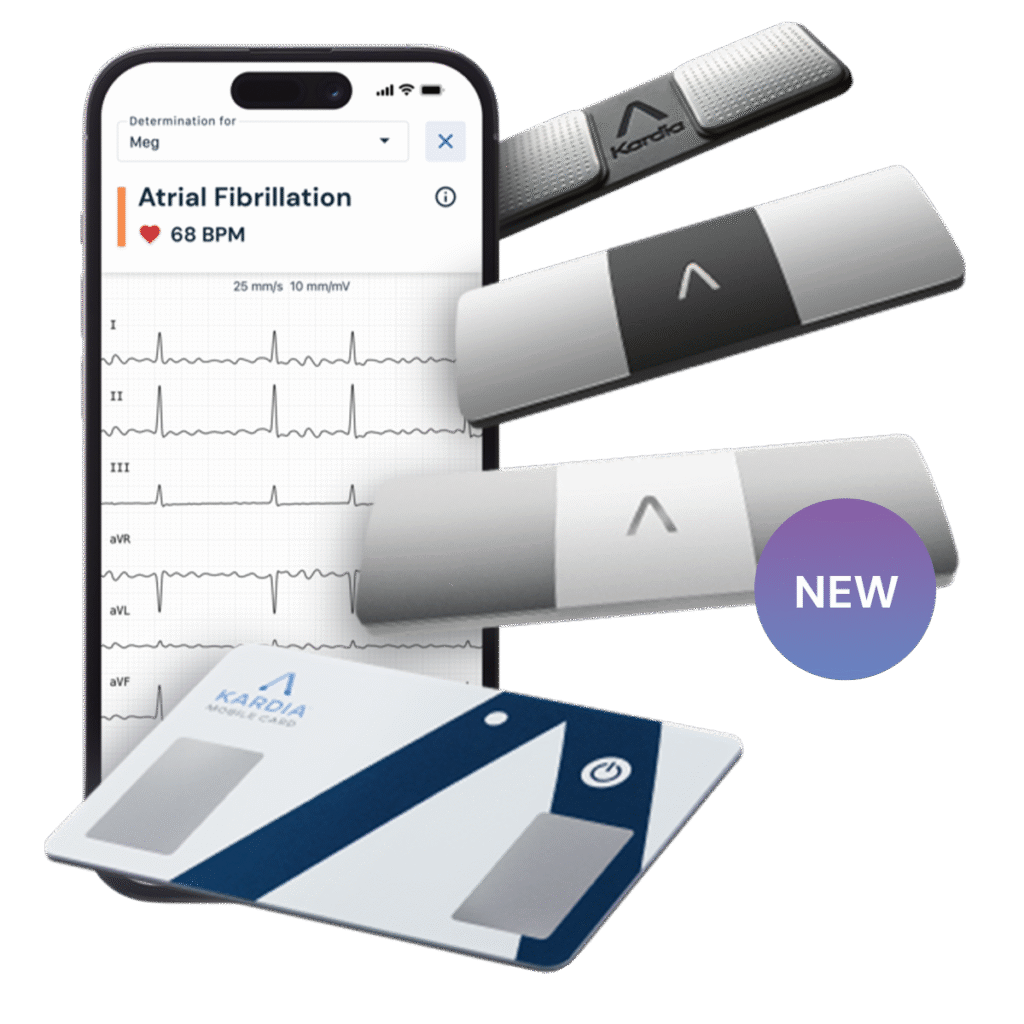
The field of imaging for atrial fibrillation is on the brink of groundbreaking innovations. Technologies like wearable devices for continuous heart rhythm monitoring are already emerging.
Recommended Heart monitoring devices:

Stay informed with the latest research and resources to help manage atrial fibrillation.
Integration with AI and Telemedicine
The future of interpreting atrial fibrillation images looks promising with AI integration. These algorithms will be able to learn from vast datasets, enhancing their ability to detect subtle changes and patterns that might be missed by the human eye. Additionally, telemedicine platforms can facilitate remote monitoring, providing continuous feedback on patients’ heart rhythms. This approach can lead to timely interventions and improved management of atrial fibrillation.
Manage Atrial Fibrillation
Learn about atrial fibrillation, its risks, and how to manage this common heart rhythm disorder effectively for better health.